Lecanemab, an investigational new drug for Alzheimer’s disease, has shown encouraging results in treating the disease, according to the expected results of a clinical trial recently presented by Eisai and Biogen, the two companies that developed it. The drug appears to have slowed the evolution of patients’ cognitive problems in the early stages of the disease, but it also led to adverse effects such as accumulation of fluid in the brain and cerebral hemorrhage. The results were communicated in very positive tones by the two companies, but many experts call for caution and remind that further investigations will be needed on the efficacy and safety of lecanemab.
Currently available drugs try to treat the symptoms of Alzheimer’s, but are not very effective against the disease, especially in its more advanced forms. For this reason, various research groups have been working for some time to try to intervene on the causes of the disease – which, however, are not yet completely clear – to make it progress more slowly.
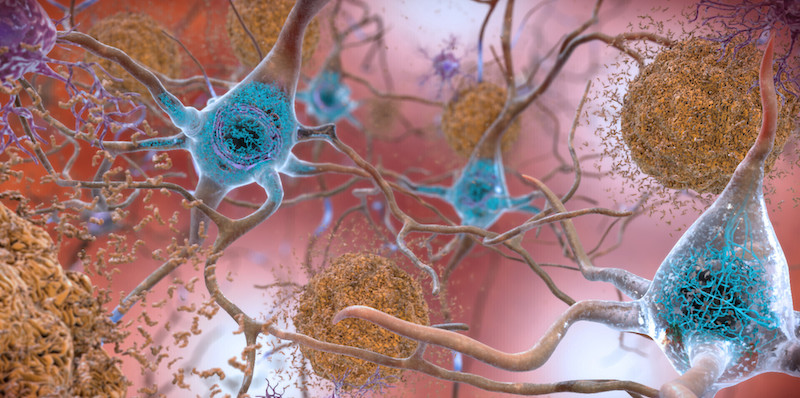
Research has focused on betamyloid, a protein that causes an accumulation of plaques in neurons (brain cells), making them gradually less reactive and functional. This protein is suspected to be one, if not the main cause of Alzheimer’s, but keeping it under control is very difficult and there are still questions about its role in the disease. Drugs such as lecanemab therefore do not have the objective of curing Alzheimer’s or of reducing the effects that have now manifested themselves, for example with a significant loss of the cognitive abilities of a sick person.
A report on the clinical study of the new active ingredient has been published in the scientific journal New England Journal of Medicine, with information on the data collected in 18 months of experimentation. According to the authors, the administration of the drug resulted in a “less decline in measures of cognitive and functional abilities” compared to participants who had received a drug that does nothing (placebo).
The trial involved 1,800 people with mild symptoms of Alzheimer’s, in order to verify the effectiveness of the treatment in the early stages of the disease. The research team reported that patients who received lecanemab experienced a decline in cognition 27 percent slower than patients receiving placebo; on the scale to evaluate the progress of cognitive abilities it is equivalent to about 0.45 points out of a total of 18.
It is the first time that a clinical trial with a drug against beta amyloid indicates a slowdown in cognitive decline: however, the reduction is not very marked and consequently doctors and experts are wondering if it could be sufficient to be noticed by patients and their loved ones. The difference compared to placebo is also not very significant, so one wonders whether treatments of this type, which can cost tens of thousands of dollars, lead to clinically meaningful benefits.
An analysis of the risk of any adverse effects must also be included in the evaluation of the drug’s benefits. Six deaths among 898 people who received lecanemab and seven deaths among patients who received a placebo were reported in the recently published report. No deaths were considered attributable to the administration of lecanemab or to episodes of cerebral hemorrhage or edema, which can occur with drugs that affect beta-amyloid.
In recent months, however, there had been a lot of talk among insiders about lecanemab following the news of the death of two patients from edema and cerebral hemorrhage. Both deaths occurred outside the 18-month clinical trial period and are therefore not included in the newly published report. It is also not known whether the people involved had taken the actual drug or the placebo during the trial, although at the end of the 18 months they had both chosen to receive the actual drug by participating in a clinical trial extension (a practice that is often done to collect more data on the efficacy and safety of a treatment).
One of the two people who died was a man in his eighties who had been taking anticoagulants to thin the blood for some time to control some heart problems. Before his death, he had been injured following several falls and had a transient ischemic attack (TIA, a stroke of moderate intensity and duration) shortly before his death. The other patient was a 65-year-old woman who had had a stroke treated with anticoagulants, before suffering a massive brain hemorrhage which eventually caused her death. According to the autopsy, lecanemab had probably weakened some blood vessels that had not then held up to anticoagulant therapy.
Eisai had issued a statement citing some analyzes conducted on the clinical histories of the two patients, concluding that the deaths could not be attributed to the intake of lecanemab, conclusions that were greeted with concern by various experts. In the clinical trial, 13 percent of patients treated with lecanemab had mild or moderate brain edema depending on the case, compared with 2 percent among those taking the placebo. In most cases, however, the edemas did not lead to particular symptoms and resolved after a few months. In contrast, 17 percent of the patients had cerebral hemorrhage, compared with 9 percent of those who received the placebo.
The most serious adverse events occurred in 14 percent of the lecanemab patients and 11 percent in the placebo group. Just under 7 percent of the participants in the trial with the actual drug dropped out of the trial due to adverse effects, about twice as many as those given the placebo. After the intravenous infusion, which is given every two weeks, some patients had reported flu-like symptoms which decreased during treatment with subsequent infusions.
At the beginning of 2023, the Food and Drug Administration (FDA), the US federal agency that deals with drugs, will have to decide whether to grant an accelerated approval path for lecanemab, in order to make it quickly available to patients. In this case, Eisai and Biogen will have to proceed with further clinical trials to demonstrate the benefits of the drug, in order to receive the necessary authorizations.
The approval process could be similar to that of aducanumab (whose trade name is Aduhelm), approved by the FDA in June 2021 and which has not led to the desired results. Already at the time, the approval had been accompanied by many doubts about its effectiveness and the very ways in which it had been approved, despite the lack of convincing evidence on efficacy and risks. A year and a half after its approval, aducanumab is little used and could end up in the long list of drugs developed with enormous investments and which have then led to disappointing results.
Leading pharmaceutical companies invest the equivalent of hundreds of millions of euros each year to develop and test new molecules, in search of the most promising candidates for obtaining new-generation drugs effective against Alzheimer’s. In 20 years of research, despite the numerous innovations and the availability of new discoveries, no drugs have emerged that have constituted a turning point for keeping the disease under control, which usually manifests itself after the age of 65 with early symptoms such as to remember recent events. Symptoms worsen with advancing age, with disorientation, sudden mood swings, depression and increasing difficulty remembering.