One of the emergencies that experts will have to deal with more and more in the coming years is age-related macular degeneration, which currently affects over 1 million Italians who have a “hole” in the center of their visual field: for them, reading is almost impossible, driving a utopia and also walking and going to the shops a feat. A panorama destined to change in the near future thanks to the arrival of new drugs and innovative intervention strategies on which experts will take stock during the second National Congress of the Italian Society of Ophthalmological Sciences. “Maculopathy is a pathology that significantly compromises the quality of life of patients and is very widespread: it affects 2% of Italians and increases with age – observes Stanislao Rizzo, director of the Ophthalmology Clinic of the A. Gemelli University Hospital IRCSS, full professor of Ophthalmology at the Catholic University and member of the SISO board of directors – It is now a social disease and represents the most frequent cause of low vision and visual impairment after the age of 50 in the Western world. There are two forms, the “dry” one, the most common (about 90% of all forms), and the wet or exudative one. Up until a few years ago, wet maculopathy was not considered curable, but the therapeutic advances of recent years have made it possible to considerably slow down its progression and reduce its evolution”.
Late diagnosis
“Unfortunately – warns the expert – many patients arrive at the diagnosis late because they do not undergo eye checkups after the age of 50 and because they neglect the initial symptoms, mainly consisting of a slightly distorted vision of the images: if the The other eye is healthy, it happens that you don’t notice it right away and the disorder progresses, until you get to the appearance of a potentially irreversible and indistinct dark spot in the middle of the visual field. The goal of research in recent years has therefore been to find drugs that could be more effective in delaying the progression of visual loss by also acting on other growth factors involved, and that would make treatment easier, reducing the need for intravitreal administrations” . Dry maculopathy is due to the formation of yellowish deposits under the macula with atrophy of the retinal tissue and the reduction of central vision is generally more gradual and slowly progressive. EMA approval is expected this year, following the FDA’s approval a few months ago, of a new drug, Pegcetacoplan, a therapy currently in use for patients with a rare blood disease. “In patients with dry maculopathy, in the most advanced forms, currently orphaned of therapies, the drug, injected intravitreally, – explains Rizzo – goes to inactivate the mechanism of inflammation which is mediated by the “complement cascade”, i.e. a series chain of inflammatory events responsible for photoreceptor degeneration. The drug could slow down its evolution without unfortunately restoring sight. The phase I trials (Filly), II and III (OAKS and DERBY) have shown a regression of the areas of retinal atrophy in the face of good safety profiles”, underlines the expert.
The causes of maculopathy
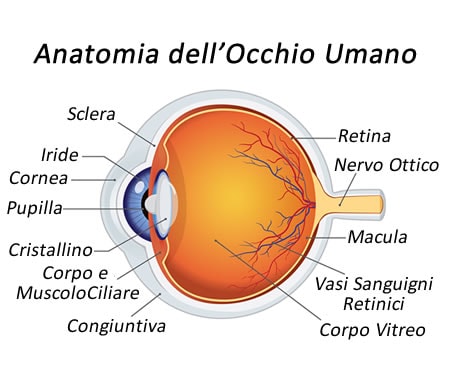
“Wet” maculopathy is caused by an abnormal growth of new vessels under the macula, the central part of the retina responsible for fine vision and vision impairment in this form can occur suddenly. The wet form therapy for some years has made use of very powerful drugs directed against a growth factor that facilitates the proliferation of new vessels in the macular region. These are the so-called anti-VEGF therapies which are administered directly into the eye (intravitreal injections) on an ongoing basis, generally once a month, with a considerable time commitment also by the patient. “However, innovative therapies are finally arriving, increasingly powerful and with a long duration of action, which will allow us to lengthen the treatment intervals”, declares Francesco Bandello, director of the Vita-Salute San Raffaele Ophthalmology Clinic in Milan and member of the SISO Board of Directors “ This is the case of the new faricimab antibody, which has been available for a few months and will soon be reimbursable by the National Health Service. This is the first bispecific antibody, i.e. with a “double target” because in addition to acting as an anti-VEGF it also affects a second important target, i.e. angipoietin-2, another substance which helps to increase the formation of new vessels, contributing to this way to improve vascular stability and reduce vessel response to VEGF”. Also in Italy, again in 2023, against wet senile maculopathy and diabetic macular edema, an already used anti-VEGF monoclonal antibody, ranibizumab, inserted in a small refillable tank, implanted in the wall of the eye and which delivers small daily amount of drug.
The innovative therapeutic strategy
“The innovative therapeutic strategy is to surgically implant small reservoirs in the eye that gradually release the drug inside. This could extend the reprocessing interval to six months, simply by refilling the tank and thus reducing the number of injections needed per year”. The data show that almost all patients (98%) can allow an interval of 6 months to pass between one refill and the next, with the same therapeutic efficacy as the monthly intravitreal treatment of the drug. Also with regard to the use of faricimab, recent studies also published in The Lancet confirm that in 60% of patients it can be administered every 4 months, instead of 2 as the current standard of care. The new treatments therefore add an advantage: the extension of the interval between administrations, reducing the number of injections. Gene therapy is the most advanced therapy, it is a great resource for the treatment of some rare retinal pathologies, and it is becoming increasingly popular. “It is now consolidated and approved – says prof. Rizzo – gene therapy for one form of inherited retinal dystrophy, Leber congenital amaurosis (LCA), while clinical trials are currently underway with gene therapy for other variants of retinitis pigmentosa, Usher syndrome, and Stargardt disease . These are diseases for which researchers have managed to identify a specific “defective” gene that prevents certain retinal cells from functioning properly, causing vision problems that can get worse over time. With gene therapy, these “defective” genes are replaced with healthy copies, thus correcting the error that triggered the disease, potentially for life.
The progress of science
Thanks to advances in science and medical technology, gene therapy will soon be able to be used against some serious eye diseases and not just to correct hereditary diseases. “A gene therapy for the treatment of wet senile maculopathy, diabetic retinopathy and other chronic retinal diseases is also under study. In these cases it is not a question of replacing a diseased gene or correcting a defect, but of modifying the genome of the retinal cells causing them to produce anti-VEGF substances, the same drugs that we have so far injected from outside once a month”. New possible applications for the diagnosis of retinal pathologies could come from the use of artificial intelligence. In an Italian clinical trial, conducted in Piedmont, the effectiveness of a specific algorithm, Dairet (Diabetes Artificial Intelligence for RETinopathy), was demonstrated for the first-level screening of diabetic retinopathy, a complication that affects 30% of diabetic patients. The study, published in the Diabetes & Obesity International Journal, demonstrated a high efficacy of the algorithm in detecting mild and moderate cases of retinopathy, with a sensitivity ratio, i.e. the ability to identify cases, equal to 91.6 % for mild retinopathy and 100% for moderate retinopathy. The specificity of the test, i.e. the ability to correctly identify healthy subjects, was also very high, with a specificity ratio of 82.6%, therefore with a low false positive rate.
Follow ilfogliettone.it on facebook
© breaking latest news