Fonte: EY, How will you design information architecture to unlock the power of data?
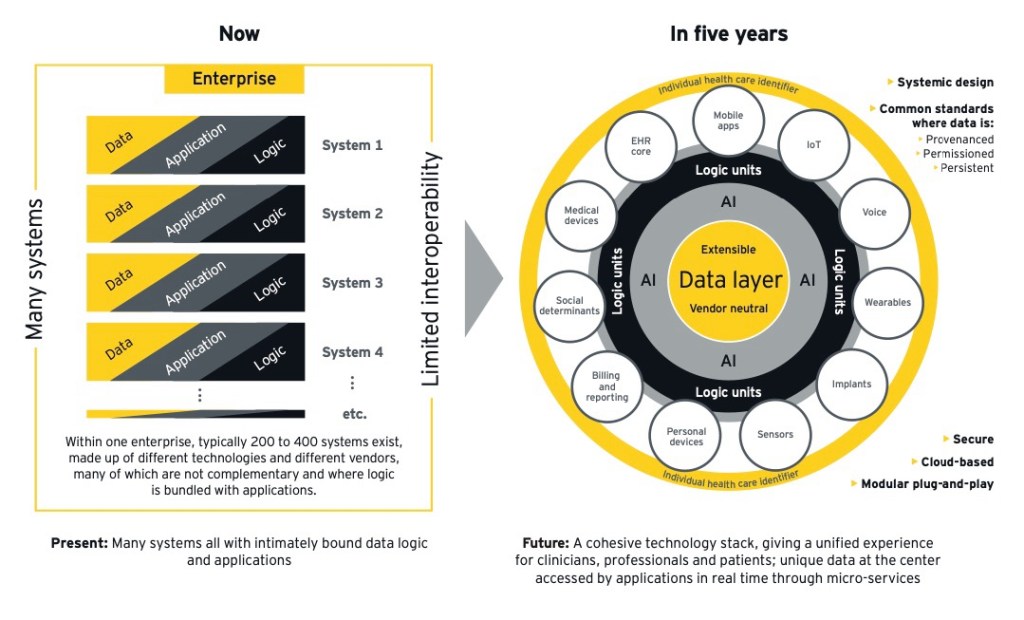
Data today is an integral part of applications and therefore fragmented and duplicated between different systems. Interoperability is a workaround but not the solution to solve this problem.
Most healthcare software applications are based on “app-centric” architectures in which data is stored as an integral part of the application itself, each of which is responsible for storing, protecting, verifying and sharing the information that manages.
Even the encodings that the application uses are an integral part of the data which are almost always in a closed and proprietary format, just as the functions and forms are inside the code and there is almost never a workflow logic; events are handled in code.
Health information systems, as we know, are made up of dozens if not hundreds of different applications. This situation determines four important consequences:
The fragmentation and duplication of data The need, to ensure that all these applications talk to each other, to pursue interoperability between systems, a very complex and demanding aspect The need, as any aspect involving data, functions or flows varies of work, of putting the code to work, a task that requires technical resources and time. The resulting strong lock-in of the supplier.
It must be noted that, to overcome this criticality, it is not at all sufficient, as many specifications require, to possess the license or even the source codes (perhaps I will return to this in an ad hoc article).
The presence of many data silos also creates another problem: the hard and difficult work when you need to replace an application and migrate its data.
For all these reasons it is useful to think about moving from an application-centric architecture to a data-centric one. This step eliminates data silos, eliminates point-to-point integrations between applications, and provides a composite architecture that accelerates development.
And document of EY on information architecture illustrates this concept very well with the following diagram.
Fonte: EY, How will you design information architecture to unlock the power of data?
Healthcare organizations considering this change will need to carefully consider how to manage their data, especially if this will be at the center of their architecture, since this is a strategic and long-term decision, which is why it is important not to be tied to one single supplier.
It must also be considered that since they will have to manage complex healthcare data, an approach will be needed that manages this complexity and allows the information to be precisely defined. They will then need to build an ecosystem of applications around the data, so they will need a robust modeling framework that encourages agility and reuse.
openEHR addresses each of these considerations as a fundamental part of its design. It has an open architecture, allowing patient-centered information to be stored in a long-lived, vendor-neutral format with version management. Secondly, it has a semantic architecture that allows you to precisely define the meaning of health and care information. Finally, it has a robust modeling framework, where domain models are created by domain experts (such as doctors) and are separated from technical layers, which leads to greater agility and reuse.
A data-centric approach – implemented with openEHR – will enable the emergence of an ecosystem of intuitive, user-centric applications. Furthermore, it will enable innovation in clinical research, digital therapeutics, disease prevention and population health management, leveraging complementary standards such as FHIR, OMOP CDM and models such as Data Mesh.
There are many examples of adoption around the world. Perhaps the most recent and high-profile example is that of the Catalan Health Service. The Health Service of Catalonia intends to use openEHR for its new health record platform across the region. The announcement highlights that the current information sharing system is a “obstacle to the systematic use of health data“, con “semantic interoperability which is probably the biggest problem“.
A shared care planning solution has been implemented in London through a persistent data platform with openEHR coupled with a low-code environment for health and care professionals to dynamically evolve digital care planning services.
In Wales, Digital Health and Care Wales (DHCW) has announced a contract to implement a clinical data repository which will be a “integral part” of national architecture and “will help transform patient care and treatment“.
In Slovenia, the Slovenian Ministry of Health has been using openEHR since 2012, creating national interoperability services across the country. In the city of Moscow, more than 670 healthcare providers use an openEHR platform to manage the health and social care records of more than 12.6 million citizens.
In the NHS, the latest “Data Saves Lives” strategy commits to “separate the data layer from the application layer [per fornire] a set of standardized… clean data“.
But how is it possible to address this paradigm shift? What is the path to take?
We’ll talk about it in the next article. Stay connected!
I like:
I like Loading…