Introduction
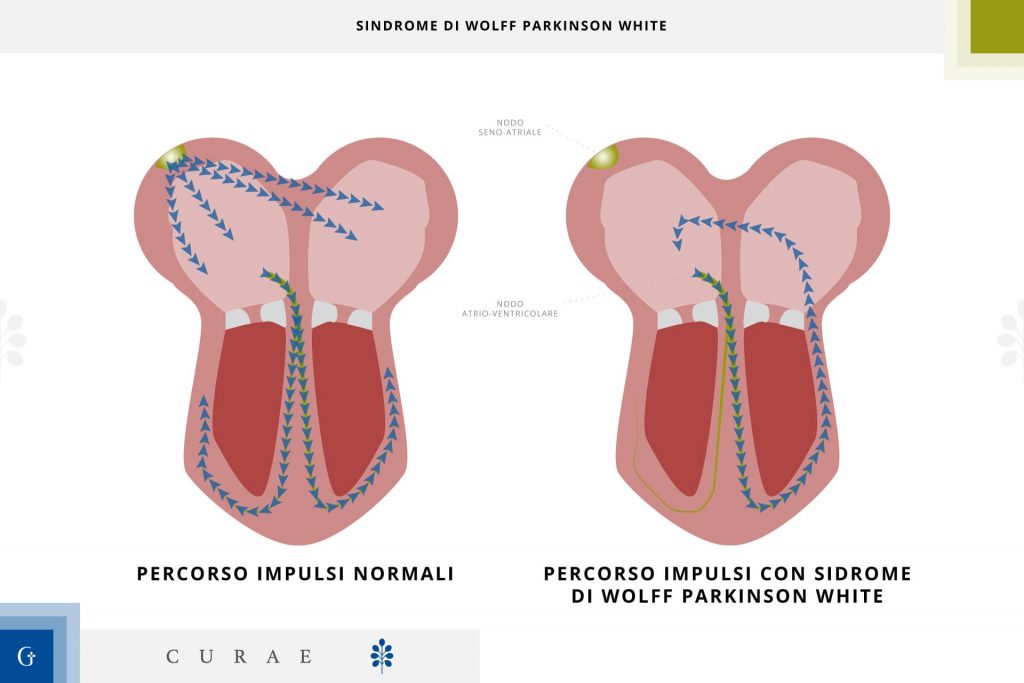
Wolff-Parkinson-White syndrome it is a disease in which an accessory pathway between the atria and ventricles is present from birth. Patients may have episodes of very fast heartbeat.
Most patients are aware of heartbeats (palpitations), and some complain of weakness or shortness of breath. The electrocardiogram is used to make the diagnosis. Usually, episodes can be resolved with maneuvers aimed at stimulating the vagus nerve, which slows the heart rate.
This syndrome is the most common of the various disorders involving an extra (accessory) electrical pathway between the atria and the ventricles. (Such disorders can produce atrioventricular reciprocating supraventricular tachycardias.) The accessory pathway makes abnormal heart rhythms (arrhythmias) more likely to develop.
Advertisements
The abnormal pathway that causes Wolff-Parkinson-White syndrome is congenital, but the arrhythmias it causes usually only appear during the teens or early 20s. However, arrhythmias can occur during the first year of life or after age 60.
Symptoms of WPW syndrome
Wolff-Parkinson-White syndrome is a frequent cause of paroxysmal supraventricular tachycardia. Very rarely, this syndrome causes an extremely rapid and life-threatening heart rate during atrial fibrillation.
If children develop arrhythmias due to this syndrome, they may be short of breath, drowsy, lose appetite, or have rapid, visible chest throbbing. Heart failure can occur.
When adolescents or people under the age of 25 develop arrhythmia due to this syndrome, it usually presents as palpitations, which begin suddenly, often during exercise. They can last only a few seconds, as well as persist for many hours. For the majority of patients, a very fast heart rate is annoying and concerning. In some cases, fainting occurs.
When episodes of paroxysmal supraventricular tachycardia due to Wolff-Parkinson-White syndrome occur later in life, they usually cause more symptoms, such as fainting, shortness of breath, and chest pain.
Atrial fibrillation and Wolff-Parkinson-White syndrome
Atrial fibrillation can be especially dangerous for people with Wolff-Parkinson-White syndrome. The accessory pathway can conduct rapid impulses to the ventricles at a much faster rate than the normal pathway (through the AV node). The result is an extremely rapid and potentially lethal ventricular rate. Not only is the heart inefficient when it beats so fast, but such a fast heart rate can also turn into ventricular fibrillation, which can be lethal if not treated quickly.
Diagnosis of WPW syndrome
Because Wolff-Parkinson-White syndrome changes the way electrical firing occurs in the heart, it can be diagnosed by an electrocardiogram (ECG), which records the electrical activity of the heart.
Treatment of WPW syndrome
Maneuvers and drugs to convert heart rhythm Sometimes ablation
Episodes of paroxysmal supraventricular tachycardia due to Wolff-Parkinson-White syndrome can often be resolved by one of several maneuvers that stimulate the vagus nerve and thereby reduce the heart rate. The maneuvers are
Strain as if it is difficult to defecate Rub the neck just below the jaw angle (to stimulate a sensitive area of the carotid artery called the carotid sinus) Place the face in a bowl of ice cold water
Such maneuvers are most effective soon after the onset of the arrhythmia.
If these prove ineffective, drugs such as verapamil or adenosine are usually given intravenously to stop the arrhythmia. Therapy with antiarrhythmic drugs can then be continued indefinitely, to prevent new episodes of tachyarrhythmia
Usually, in infants and children younger than 10 years, digoxin can be given to suppress episodes of paroxysmal supraventricular tachycardia due to Wolff-Parkinson-White syndrome. However, adults with this syndrome should not take digoxin because it can facilitate conduction along the accessory pathway and increase the risk that atrial fibrillation will cause ventricular fibrillation. For this reason, digoxin is usually stopped before people with the syndrome reach puberty.
Ablation
Partial destruction of the accessory pathway by catheter ablation (delivery of energy using radio waves, laser pulses, or a high-voltage electrical current, or freezing through a catheter inserted into the heart) is successful in over 95% of cases. The risk of dying during this procedure is less than 1 in 1,000. Ablation is particularly useful in young patients who might otherwise be forced to take antiarrhythmic drugs for life.
NurseTimes editorial team
Fonte: Manuale MSD
Image: www.policlinicogemelli.it
Stay up to date with Nurse Times, follow us on:
Telegram – https://t.me/NurseTimes_Channel
Instagram – https://www.instagram.com/nursetimes.it/
Facebook – https://www.facebook.com/NurseTimes. NT
Twitter –